August 2013 – Amid an increasing cancer burden and limited pathology services, a new pathology lab in Lilongwe, Malawi provides a robust platform for cancer care and research.
Early Experience after Developing a Pathology Laboratory in Malawi, with Emphasis on Cancer Diagnoses
Satish Gopal, Robert Krysiak, N. George Liomba, Marie-Josephe Horner, Carol G. Shores, Noor Alide, Steve Kamiza, Coxcilly Kampani, Fred Chimzimu, Yuri Fedoriw, Dirk P. Dittmer, Mina C. Hosseinipour, Irving F. Hoffman
PLoS One
Full text available at PubMed Central and PLuS One
Abstract
Background
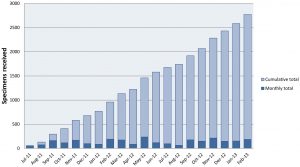
Despite increasing cancer burden in Malawi, pathology services are limited. We describe operations during the first 20 months of a new pathology laboratory in Lilongwe, with emphasis on cancer diagnoses.
Methods and Findings
We performed a cross-sectional study of specimens from the Kamuzu Central Hospital pathology laboratory between July 1, 2011 and February 28, 2013. Patient and specimen characteristics, and final diagnoses are summarized. Diagnoses were categorized as malignant, premalignant, infectious, other pathology, normal or benign, or nondiagnostic. Patient characteristics associated with premalignancy and malignancy were assessed using logistic regression. Of 2772 specimens, 2758 (99%) with a recorded final diagnosis were included, drawn from 2639 unique patients. Mean age was 38 years and 63% were female. Of those with documented HIV status, 51% had unknown status, and 36% with known status were infected. Histologic specimens comprised 91% of cases, and cytologic specimens 9%. Malignant diagnoses were most common overall (n = 861, 31%). Among cancers, cervical cancer was most common (n = 117, 14%), followed by lymphoma (n = 91, 11%), esophageal cancer (n = 86, 10%), sarcoma excluding Kaposi sarcoma (n = 75, 9%), and breast cancer (n = 61, 7%). HIV status was known for 95 (11%) of malignancies, with HIV prevalence ranging from 9% for breast cancer to 81% for cervical cancer. Increasing age was consistently associated with malignancy [bivariable odds ratio 1.24 per decade increase (95% CI 1.19–1.29) among 2685 patients with known age; multivariable odds ratio 1.33 per decade increase (95% CI 1.14–1.56) among 317 patients with known age, gender, and HIV status], while HIV infection and gender were not.
Conclusions
Despite selection and referral bias inherent in these data, a new pathology laboratory in Lilongwe has created a robust platform for cancer care and research. Strategies to effectively capture clinical information for pathologically confirmed cancers can allow these data to complement population-based registration.