If health equity is at the core of global health, practice begins where we put our feet. Health disparities can be intensely local and this includes many populations in North Carolina. The Institute strives to achieve optimal health for the most vulnerable populations, with practice that expands education and training across fields and professions. The Wake County Health and Human Services Infectious Diseases and STI Clinics successfully demonstrate service-engaged work, a 25-year collaboration between UNC Infectious Diseases and Wake County.
In March 2020, while many clinics were closing down because of COVID-19, the Wake County Infectious Diseases Clinic–a community HIV services organization funded by Wake County, with case management and links to care and bridge counseling–stayed open. The healthcare providers, nurses and staff continued to care for uninsured patients, advocating for those who sometime need to go through the full spectrum of their emotions, to feel safe and trusted, before getting to the heart of their visits.
This is a place where service is the synthesis of transformative clinical research that positively changes global health outcomes, where a staff member might use the lunch hour to drive to a pharmacy for a patient’s refill, because the patient isn’t able to get there, then dropping it off at his apartment because it’s so important to stay on treatment. This is a place where workers are guided by a strong moral compass, and it can be exhausting, says Chris Evans. But at the same time, knowing that patients are being helped makes it all worthwhile.
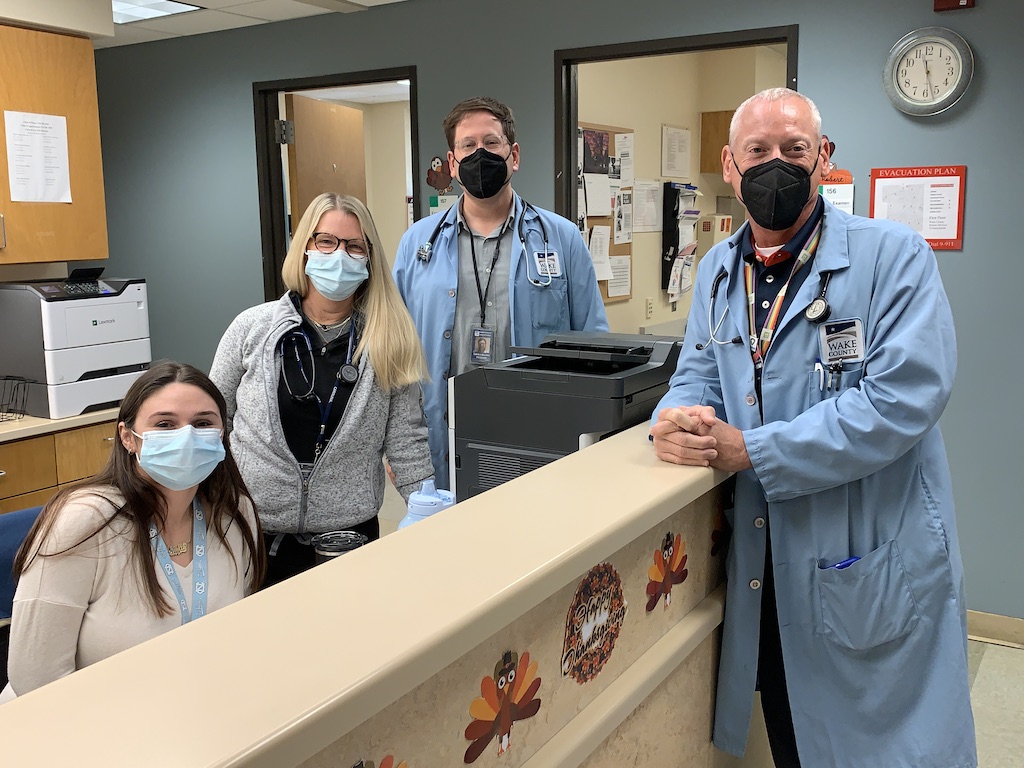
The Wake County Infectious Diseases and STI Clinics
The Wake County Infectious Diseases and STI Clinics are located at 10 Sunnybrook Road in Raleigh, North Carolina. The Infectious Diseases/HIV Clinic (Clinic B) provides primary care, funded by Ryan White Part B/C funds. The STI Clinic (Clinic A) provides PEP/PrEP and Hepatitis C treatment, but also includes prevention and treatment of STIs, funded by County/State/Federal.
Staff are employed by both UNC and Wake County, with grant funding that provides clinical revenue. Christopher Sellers, MD, MPH, is Medical Director of the Wake County Health and Human Services Infectious Diseases and STI Clinics. Robert Dodge, PhD, RN, ANP, AACRN, FAANP, is the Clinic Director, who has worked at the clinic for 21 years, and manages the Ryan White Part C grant. Others include Kathryn Watson, MSN, RN, AGNP-C; Chris Evans, DNP, RN, ANP; Elizabeth Moore, PhD, MSc, FNP-BC; Elizabeth “Eli” Arant, MD; and Jackie Gibson, PA-C. Victoria Mobley, MD, MPH, a state medical epidemiologist and previous UNC ID Fellow, is the Medical Director for the NC Division of Public Health. She is a frequent volunteer, often working in the evenings.
Drs. Sellers, Dodge and Evans describe how they serve patients and what they enjoy about their work, in the following interview.
How did these clinics start?
Robert Dodge: “This is a partnership between UNC and Wake County that started in the early 1990s, housed with UNC because it has always had a public health service component, compared to other healthcare organizations. Wake County is a large populous county that had a significant number of people living with HIV for a long time, who needed accessible care and support services.”
Christopher Sellers: “Our infectious disease experts were at the forefront of the epidemic in Chapel Hill, while doing national research and starting treatments. UNC had the Francis Owen Blood Center that spurred early engagement with HIV. There were more people getting diagnosed in Chapel Hill and there was more medical care to give patients, which became funded by the Ryan White Act. These were some of the factors that led to the clinic’s existence.”
Chris Evans: “During the HIV/AIDS epidemic, Wake County needed assistance managing it. UNC’s emerging HIV program was led by Dr. Myron Cohen and now by Dr. Joe Eron. We’re really proud of the work that’s been done and what we continue to do.”
How has patient care grown?
Christopher Sellers: “We have a relatively new PEP/PrEP Clinic, which is nested in the STI Clinic, that we built from the ground up five years ago, based on seeing how many patients were coming through as HIV negative patients in the STI Clinic, who would benefit from PEP/PrEP, and the really limited availability of PEP/PrEP resources for uninsured patients. It does a good job reaching directly into a population that a lot of times doesn’t have any other contacts with the health system.
“Along those lines, we started a much smaller but active Hep C Treatment Clinic because we would diagnose people with Hep C, as part of routine screening during STI visits. We wouldn’t have anywhere to refer them, where they were likely to get treatment. So, this clinic treats a really high-risk population that doesn’t have contact with the medical system, as well as people who are really high risk, passing Hep C through IV drug use or having untreated Hep C. There are not many Hep C treatment clinics in publicly funded STI Clinics, and this is a unique feature in the UNC-Wake County collaboration.
“One area we’re working to improve is mental health as it relates to adolescents. Many continue to do their visits through telehealth, which started during COVID. The data shows that by keeping these mental health appointments, they are staying stable with their mental health treatment which means they are keeping their other clinic appointments, getting their refills and staying on therapy–all of which helps to keep HIV suppressed.”
Tell us about the patients you follow?
Robert Dodge: “For the Infectious Disease/HIV Clinic we’re following approximately 1,609 patients, and we have an 85.9% viral suppression rate. For the STI Clinic, where we’re treating patients with PrEP, we have close to 500 patients.”
Christopher Sellers: “These are people who are underserved. And the reality for these patients is that because they have HIV and are coming to our clinic, they are also getting primary care they would not otherwise get anywhere else. Since I’m seeing them for primary care, they’re finally getting their diabetes managed appropriately, for example. A majority of these people may have been going to the ER and getting a bandaid for their conditions.”

How does the clinic contribute to research?
Christopher Sellers: “We’re a subunit of the Institute’s Clinical Trials Unit (CTU). Our patients participate in HIV research and they are screened here in the clinic. We’re nimble in being able to implement new therapies and state of the art approaches to care. We not only work closely with the Division of Infectious Diseases and the CTU, we work with other groups conducting HIV research. We’re a source of diverse research subjects and people who want to participate, who are sometimes harder to reach in clinical research.”
How would you describe the patients.
Christopher Sellers: “In general, people living with HIV in the US are disproportionately affected by a lot of things that make it harder to access care. As such, we have a higher proportion of people who are very low income, with unstable housing and things like that. Everyone from people who are incarcerated for prolonged periods of time to people who are homeless.”
Chris Evans: “We see some patients who are really quite sick, that need a lot of attention and care, while others are in a maintenance phase. Food and housing insecurity impact a lot of our patients. We do a lot to help them with the basics, like navigating pharmacies in the healthcare system.”
What do you like about working at the clinic?
Christopher Sellers: “It can be challenging but it can also be inspiring. I think everyone really believes in what they’re doing and that makes for a nice place to work. We’ve had lots of success due to the talents of the people working here, and every role that contributes to providing really good care, ultimately translates into high rates of viral suppression. Sometimes, the hardest parts of our work are the situations that we don’t have training for, that aren’t in our skill set. There are lots of examples of people doing good work in that regard.”
What’s a typical day like at the clinic?
Chris Evans: “It varies from day to day but on average we could see 12 or 14 patients a day, and some are quite complicated. There are many challenges around unstable housing and data shows if someone has unstable housing, adherence to treatment and viral suppression is directly impacted. There are visits with patients who just need to feel safe.”
How does the clinic provide training opportunities?
Christopher Sellers: “All of the UNC ID fellows rotate through the STI and PrEP Clinics as part of their STI rotation. They all come out and work with us, which we benefit from and enjoy. There’s also a full rotation of fourth year pharmacy students in the Infectious Diseases clinic, who can do a community HIV clinic rotation, Chris Evans is the preceptor, and we’re a training site for Wake Med which has an ID pharmacy residency. So, there’s always an ID pharmacy resident who spends time with us and gets experience in the Infectious Diseases clinic. We also frequently host students from the UNC PA Program, the UNC School of Nursing and other universities like Duke and ECU.”
What healthcare innovations are you working on?
Christopher Sellers: “Michael McNeill, the grants manager for our clinic in charge of the Ryan White Region 6 Care Network, has been instrumental in setting up a medical Uber program that’s been funded. This is really helping patients who struggle to get to clinic because of transportation.
“We’ve also piloted a new two-way texting program as a facilitator of engagement and care that will be expanding. This is through a HRSA grant that Dr. Lina Hovee-Rosengren wrote, which will provide further access for patients in nontraditional ways. We’re nimble enough. We have lots of patients but fewer providers than the UNC ID Clinic, so it’s easier to test innovations like this.”
Chris Evans: “We care about the patients and we want them to succeed and do well. We’re willing to be creative and innovative, and think outside the box to pull that off for them.”
