A student research team led by Victor Arahirwa, a 2024 MD Candidate, received the Harold C. Pillsbury, MD Student Research Award for Excellent Poster Presentation (Clinical Science) during the recent John B. Graham Medical Student Research Society’s Annual Student Research Day.
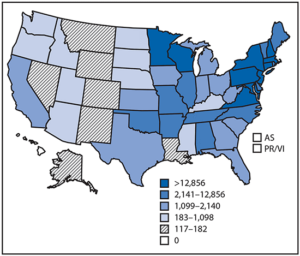
From 2004 to 2016, the Centers for Disease Prevention and Control (CDC) reported nearly 500,000 cases of tick-borne disease (TBD) occurring in the continental United States. North Carolina experiences some of the highest rates of tick-borne Rickettsia and Ehrlichia, often accounting for over 10% and 5% of national totals, respectively.
The “Impact of the COVID-19 Pandemic on the Diagnosis and Management of Tick-Borne Diseases Endemic to North Carolina” sought to examine how the COVID-19 pandemic may have contributed to changes in the management of TBDs.
“I wanted to conduct this study because I had noticed that there were delays in diagnosis and treatment for a number of conditions during the COVID-19 pandemic,” said Arahirwa. “I suspected that the patterns would hold true for tick-borne diseases in North Carolina, but I was surprised by the lack of research in this area.”

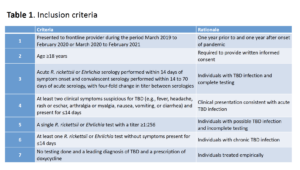
The study team initially identified patients with suspected Rocky Mountain spotted fever (RMSF) or ehrlichiosis who were seen at any UNC Health facility. Potentially eligible records were reviewed in further detail with eligible cases (Table 1) classified as either “pre-COVID” or “post-COVID” depending on the date of the reported illness. The team then documented information about how long it took patients to get a diagnosis or start treatment, comparing the pre- to the post-COVID period. They also looked at how often patients with tick-borne diseases had to undergo testing for SARS-CoV-2 before other causes were considered.
 Overall, the team found that patients in the post-COVID period were more likely to experience delays in diagnosis and treatment compared to the pre-COVID period. The non-specific nature and potential overlap of COVID-19 and TBD symptoms (i.e., fever, headache) is one factor that may explain the findings. Given the heightened awareness of COVID-19 during the study period, providers may have anchored on a potential COVID-19 diagnosis on initial presentation, delaying the consideration of TBD and empiric treatment while SARS-CoV-2 testing was performed.
Overall, the team found that patients in the post-COVID period were more likely to experience delays in diagnosis and treatment compared to the pre-COVID period. The non-specific nature and potential overlap of COVID-19 and TBD symptoms (i.e., fever, headache) is one factor that may explain the findings. Given the heightened awareness of COVID-19 during the study period, providers may have anchored on a potential COVID-19 diagnosis on initial presentation, delaying the consideration of TBD and empiric treatment while SARS-CoV-2 testing was performed.
The team also observed decreased utilization of the emergency department (ED) and increased uptake of telemedicine services. Furthermore, decreased access to outpatient clinics, hesitation about going to the ED due to long waits and fears of contracting SARS-CoV-2, and increasing use of telemedicine appointments may have negatively impacted the quality of care.
“Their work demonstrates how the pandemic adversely impacted the timely diagnosis and management of tick-borne diseases, which can present with non-specific symptoms like fever, headache, and body aches that are also common manifestations of COVID-19,” said Ross Boyce, MD, MSc, assistant professor medicine and epidemiology. “Given how concerned we all were about COVID, it’s no surprise that patients with these symptoms frequently had to undergo COVID testing – sometimes multiple tests – or were limited to telehealth appointments before a diagnosis of tick-borne disease was made.”
The team did not observe any substantial changes in the severity tick-borne diseases or eventual patient outcomes, but they caution that the small number of events limits the ability to detect small differences.
“Victor undertook a very ambitious project, and together with other team members, carried it through to successful completion. While I wish I could take more credit, this was a student-led project that highlights the many talents or our medical and public health students,” Boyce said.
The team of student investigators included Katherine Tyrlik (MPH, Applied Epidemiology), Haley Abernathy (PhD, Epidemiology), Caitlin Cassidy (PhD, Epidemiology), Aidin Alejo, (MD), Odai Mansour, (MD) Dana Giandomenico (Program Manager), and Amanda Brown Marusiak, (PhD Epidemiology).
Established in 1987, the John B. Graham Medical Student Research Society recognizes and promotes the research efforts of the medical student body at the University of North Carolina School of Medicine in the fields of basic science, public health, clinical science, medical education, quality improvement, and more. Students who participate in. Throughout the year, members exchange ideas and share their experiences about conducting research. In addition, the Society serves to encourage collaboration with faculty to promote productive research opportunities for students.
